State dental associations see wins, challenges as they advocate for dental teams to receive COVID-19 vaccine









With demand for the COVID-19 vaccine high and much of the U.S. experiencing a confusing rollout, state dental associations are advocating for dental teams in their states to be prioritized to receive the vaccine.
"The American Dental Association has deployed a three-fold strategy to support dentists — as essential health care providers — and patients: helping dentists get the vaccine; helping dentists navigate the ability to administer the vaccine; and helping dentists encourage their patients and communities to get vaccinated," said ADA President Daniel J. Klemmedson, D.D.S., M.D. "Because final authority on vaccine allocation rests with each state, we continue to work alongside state and local dental societies to advocate for dentistry before lawmakers and health departments. I understand the frustration that many dentists feel about their state's vaccine rollout, and our tripartite is working hard to advocate on their behalf."
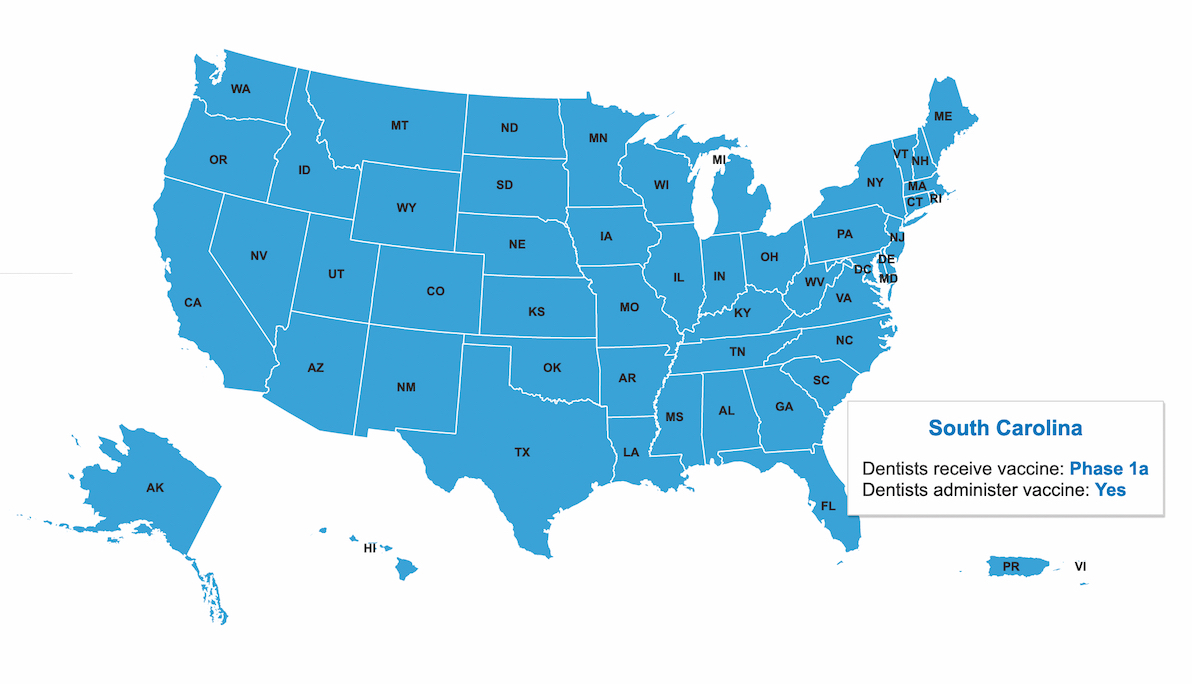
In late December 2020, the Centers for Disease Control and Prevention confirmed dental teams should be included in the first phase of the vaccine rollout with other health care personnel. Most states include dentists and their teams in Phase 1a.
"The ADA's established relationship with the CDC, and the respect that federal officials have for the dental profession, has resulted in the CDC recognizing dentists as essential health care personnel and recommending dental professionals be included in the initial phase of COVID-19 vaccine distribution," said Mark Vitale, D.M.D., vice chair of the ADA Council on Government Affairs. "State dental associations have taken the lead of the ADA and have been advocating for dentists and their teams to be included in Phase 1a."
The state associations are running into roadblocks on their way to getting dental professionals vaccinated, however, including limited vaccine supplies and a lack of communication from government agencies.
Early advocacy
In South Carolina, the state dental association played a key role in moving dentists and their clinical staff into Phase 1a of the state's COVID-19 vaccine rollout.
"Dentists were not originally included in Phase 1a. The South Carolina Dental Association had numerous meetings and sent several letters to the governor's office and other government agencies who were making the decisions, stressing the point that the dental team needed to be included in 1a," said Executive Director Phil Latham and President Julia Mikell, D.D.S. "When the CDC Advisory Committee on Immunization Practices guidelines were updated, the SCDA immediately sent that information to South Carolina’s Vaccine Advisory Committee, and within 24 hours, they moved all dental team members with direct patient contact into 1a."
While dentists have been included in Phase 1a in New York, because of limited vaccine supplies, distribution was initially restricted to frontline hospital workers and those in long-term care facilities.
"The New York State Dental Association worked with the New York State Department of Health and the governor's office to be sure the broad term 'health care personnel' included dentists and their staff," said Mark Feldman, D.M.D., executive director of the state dental association. "Vaccinations started during the last three weeks of December and, due to limited supply, were limited to those in group 1a who were frontline hospital workers and nursing home patients and staff. By week four, Jan. 4, dentists started receiving vaccination as part of group 1a due to our work with the governor's office."
In Florida, the use of the general term "health care personnel with direct patient contact" in the first phase of the rollout also caused confusion, but the state dental association helped to spread the word that dental teams were eligible for the vaccine.
"As you can imagine, there is a very large number of people included in the first phase," Florida Dental Association Executive Director Drew Eason said. "Additionally, there was a great deal of confusion county to county on who was considered 'health care personnel with direct patient contact.' We had several hospitals tell dentists, incorrectly, that they weren't eligible. We worked with the Florida Hospital Association to get the word out that dental teams are eligible."
The Idaho State Dental Association has continued to advocate to ensure its state dentists remain eligible as part of Phase 1a. Its executive director is a voting member of the Idaho COVID-19 Vaccine Advisory Committee.
"This has given us direct input into the prioritization process, enabling dentists to remain in Phase 1a of the rollout," Executive Director Linda Swanstrom said. "Getting and keeping dentists in Phase 1a was a big win, as the placement was challenged and voted on multiple times."
Dentists are included in Phase 1a in Maryland, but getting the vaccine to them was an issue when public health departments did not have their contact information. The Maryland State Dental Association helped to connect health departments and dentists.
"While the hospitals were tasked with vaccinating their own staff, in Maryland's vaccination plan, each local health department was charged with developing its own distribution plan and system. While dentistry was included in Phase 1a, access by the local health departments to contact information for dental practices was very hard to get," Executive Director Greg Buckler said. "The MSDA played a significant role in connecting the health departments to the local dental practices. Dentists’ access to the vaccine exponentially increased after the MSDA was able to serve as this conduit."
As of late January, the Texas Department of State Health Services and the state's Expert Vaccine Allocation Panel had not specifically defined when the vaccine would be available for the majority of dental health care personnel in Texas, but the Texas Dental Association has been working with state officials to get dental teams vaccinated. Some dentists have been able to receive the vaccine based on local interpretations of guidelines or hospital affiliations, and the state dental association’s local component societies have kept members updated on the availability of the vaccine in their areas.
"Texas officials continue to tell the Texas Dental Association and other stakeholders that their priority is focused on those delivering direct care to COVID-19 patients and those most negatively impacted by the virus: those 65 and older and those with conditions that impact immunities," said Matt Roberts, D.D.S., chair of the Texas Dental Association’s Council on Legislative, Regulatory and Governmental Affairs. "Regardless, the TDA continues to aggressively advocate for dentists and dental health care personnel."
Facing challenges
Overall, state dental associations have reported messy vaccine rollouts.
"Texas, like most of the nation, continues struggling to deliver COVID-19 vaccines to its identified priority groups," Dr. Roberts said. "Supply shortages, conflicting state messaging, technical errors and logistical delays all contribute to the uncertainty we are facing. Texas' vaccine supply from the federal government, distribution strategy and technical support at the state and local levels all directly impact how quickly Texas will finish vaccinating its high-risk groups."
With limited vaccine supplies and many people eligible to be vaccinated during the first phase, appointments are filling up quickly across the nation, including in New York.
"The problem is a lack of supply of vaccines with overwhelming demand," Dr. Feldman said. "Registration openings, largely done online, keep crashing, and when a site opens up, it fills up immediately. Dentists and the rest of the 1a and 1b priorities report long waits to register, and often appointments are weeks or months away. This varies, and many dentists were able to register and obtain an appointment prior to the categories expanding."
Florida has also reported long waits and crashing computer systems. While dentists and their teams have begun to receive the vaccine, appointments in some areas, particularly in the southern part of the state, are being claimed very quickly, Mr. Eason said.
"The overall rollout has been full of confusion and misinformation," he said.
While the Florida Dental Association and its local dental societies have been doing all they can to gather information for dentists, there has been minimal communication from government agencies to dentists about how to sign up for the vaccine, Mr. Eason said. With hospitals and county health departments overwhelmed, it has been difficult to reach officials there. The state dental association has let the governor’s office know of the challenges dentists are experiencing in parts of the state.
Dentists in Maryland are experiencing similar issues with a lack of communication.
"The greatest challenge dentistry in Maryland has faced with the COVID-19 vaccine is the lack of information provided throughout the process to dentists by their local health departments," Mr. Buckler said." This was compounded by a seemingly inability of various government agencies to proactively communicate among each other as the rollout transpired."
In Idaho, there was no statewide process for implementing the rollout, which led to confusion.
"We did not have a statewide centralized or consistent process for identifying the individuals in each phase, contacting them or scheduling them for vaccination," Ms. Swanstrom said. "This led to a lot of confusion early in the rollout regarding how to sign up for vaccinations and how dentists will be notified when it is time."
Dentists in South Carolina also experienced a lack of consistency, with the rollout going better in some areas than others.
"Working with numerous groups across the state has been a challenge because locations providing the vaccine operate on their own terms, and what occurs in one location may not occur in another," Mr. Latham and Dr. Mikell said.
Gaining momentum
Even with the challenges state dental associations and their dentists have experienced, things are slowly looking up, as advocacy continues and more dentists have access to the vaccine.
In Idaho, Ms. Swanstrom said the rollout is "slow, but gaining momentum."
"As supply has increased and regional health districts have gotten clear on their processes, things have improved," she said. "Across the state, dentists in Idaho now have access to and are definitely getting vaccinated, with some already receiving their second doses."
Mr. Eason also reports the rollout in Florida has "steadily improved," as dental teams in some parts of the state have been vaccinated.
But state dental associations understand the frustration dentists in their states are experiencing if they have not been vaccinated yet.
"The Texas Dental Association and our local component societies have responded to many individual questions from members," Dr. Roberts said. "We understand our members' anxiety to know when dentists can receive the vaccine, and we stand with them. That is why we are fighting for them."
State dental associations have taken pains to regularly communicate with their members about the vaccine, as well as other aspects of the pandemic.
"Our success was in keeping members updated in real time on their priority status and providing local links to register as soon as they became available," Dr. Feldman said. "Members received timely information that was not available anywhere else but from the New York State Dental Association."
For the Maryland State Dental Association, communicating with members has meant sharing updates through email and social media, presenting a webinar series about issues related to COVID-19 and creating a page on its website that serves as a one-stop shop for what dentists need to know during the pandemic, including information about getting vaccinated, Mr. Buckler said.
The advocacy provided by state dental associations has helped to positively position the associations and their dentists during the pandemic.
Because of the South Carolina Dental Association's advocacy efforts, the state's hospital association and major hospital systems were aware it was a point of contact for most dentists in South Carolina. Once the state health department moved dental personnel into Phase 1a, two of those systems reached out to the dental association to get contact information for its members.
"This provided a huge member benefit as dentists and their offices were able to register for the vaccine before our health department was able to send out communications," Mr. Latham and Dr. Mikell said. "The reputation of our association within the network we have established among other associations and agencies over the course of this pandemic paid off big time."



