ADA to hold webinar outlining new billing requirements for dentists treating Medicare beneficiaries
The American Dental Association will hold a webinar covering information for dentists wishing to treat Medicare beneficiaries and outlining other new requirements for Medicare billing set to begin next month.
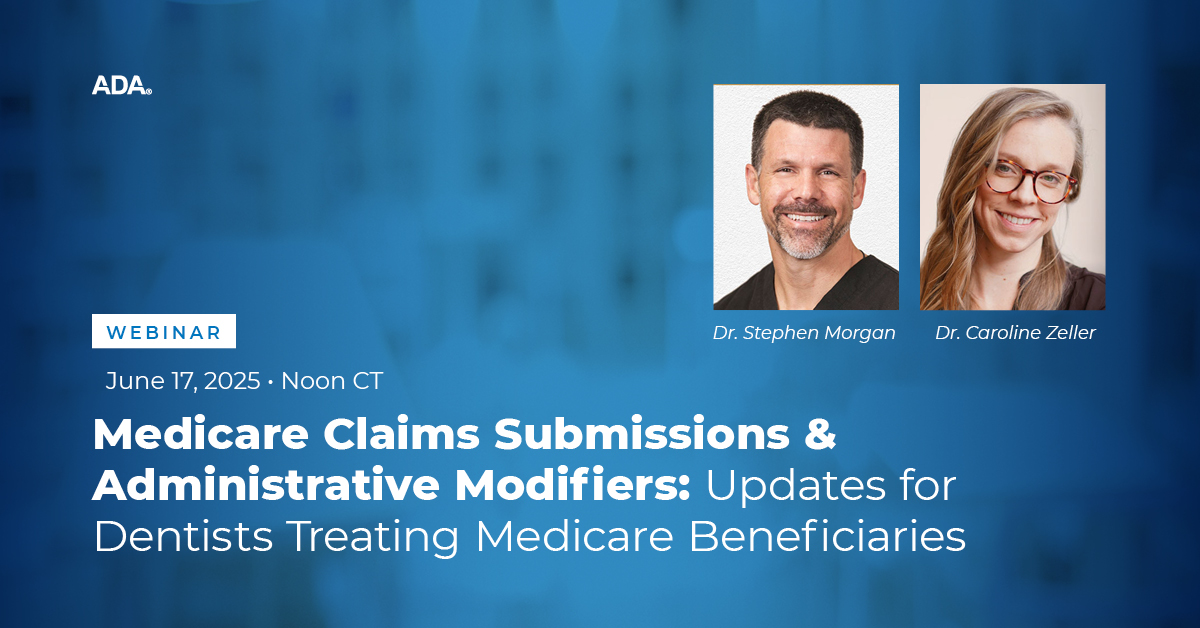
The webinar, called Medicare Claims Submissions & Administrative Modifiers: Updates for Dentists Treating Medicare Beneficiaries, will feature two member dentists who will help providers understand how to best prepare for treating Medicare beneficiaries. They are Caroline Zeller, D.D.S., member of the Council on Advocacy for Access and Prevention, and Stephen Morgan, D.D.S., chair of the Dental Content Committee and member of the Council on Dental Benefit Programs.
Beginning in 2023, the Centers for Medicare and Medicaid Services said Medicare would pay for limited dental services that were inextricably linked to the clinical success of a medical procedure. Since then, the agency has stated it will now pay for dental services linked with the following clinical scenarios:
- Dental or oral exams as part of a comprehensive workup prior to the Medicare-covered services listed below, and medically necessary diagnostic and treatment services to eliminate an oral or dental infection prior to or contemporaneously with these Medicare-covered services:
o Organ transplant, including hematopoietic stem cell and bone marrow transplant
o Cardiac valve replacement
o Valvuloplasty procedures; and
o Chemotherapy, chimeric antigen receptor (CAR) T-cell therapy, and the administration of high-dose bone-modifying agents (antiresorptive therapy) when used in the treatment of cancer. - Dental or oral exams as part of a comprehensive workup prior to medically necessary diagnostic and treatment services to eliminate an oral or dental infection prior to or contemporaneously with, and medically necessary diagnostic and treatment services to address dental or oral complications after, Medicare-covered treatment of head and neck cancer using radiation, chemotherapy, surgery, or any combination of these.
- Dental or oral examination in the inpatient/outpatient setting or medically necessary diagnostic and treatment services to eliminate an oral or dental infection prior to, or contemporaneously with, Medicare-covered dialysis services for the treatment of end-stage renal disease.
- Dental ridge reconstruction done as a result of and at the same time as surgery to remove a tumor.
- Services to stabilize or immobilize teeth related to reducing a jaw fracture.
- Dental splints, only when used as part of covered treatment of a covered medical condition such as dislocated jaw joints.
“While there are currently limited circumstances in which dental services qualify for reimbursement under traditional Medicare, it is still available to hundreds of thousands of current Medicare beneficiaries,” Dr. Zeller said. “We want to provide this education so that dentists who wish to treat Medicare beneficiaries can provide this care with fewer administrative hurdles or disruptions in a patient’s treatment.”
Slated for June 17 at 1 p.m. EST, the webinar will also provide operational information regarding billing for dual-eligible individuals and submission through electronic health records.
The Centers for Medicare and Medicaid Services’ new requirements for Medicare billing are set to begin July 1. For more information or to register, visit this webpage.



